Our law firm handles hypoxic-ischemic encephalopathy (HIE) lawsuits in Maryland. HIE is a type of brain damage that occurs when a baby’s brain doesn’t receive enough oxygen and blood, typically during or immediately before birth.
What is hypoxic-ischemic encephalopathy?
Hypoxic-ischemic encephalopathy (HIE), is a brain injury resulting from a lack of oxygen and blood flow to the baby’s brain. It can lead to seizures, difficulty feeding, low muscle tone, organ dysfunction, and breathing difficulties. HIE may cause long-term neurologic disabilities such as cerebral palsy, intraventricular hemorrhages, and learning disabilities.
What risk factors did the new study link to HIE?
There are many additional pregnancy conditions or issues that are associated with HIE. All of them involve disruption of the delivery of oxygen to the fetus.
- Nuchal cord: A nuchal cord occurs when the umbilical cord wraps around in a knot or loop around the baby’s neck. When this occurs, the cord can become obstructed, limiting the flow of oxygen-rich blood from the mother to the baby. Sometimes, it can get wound so tightly that it affects the blood vessels on the neck, depriving the baby’s brain of oxygen.
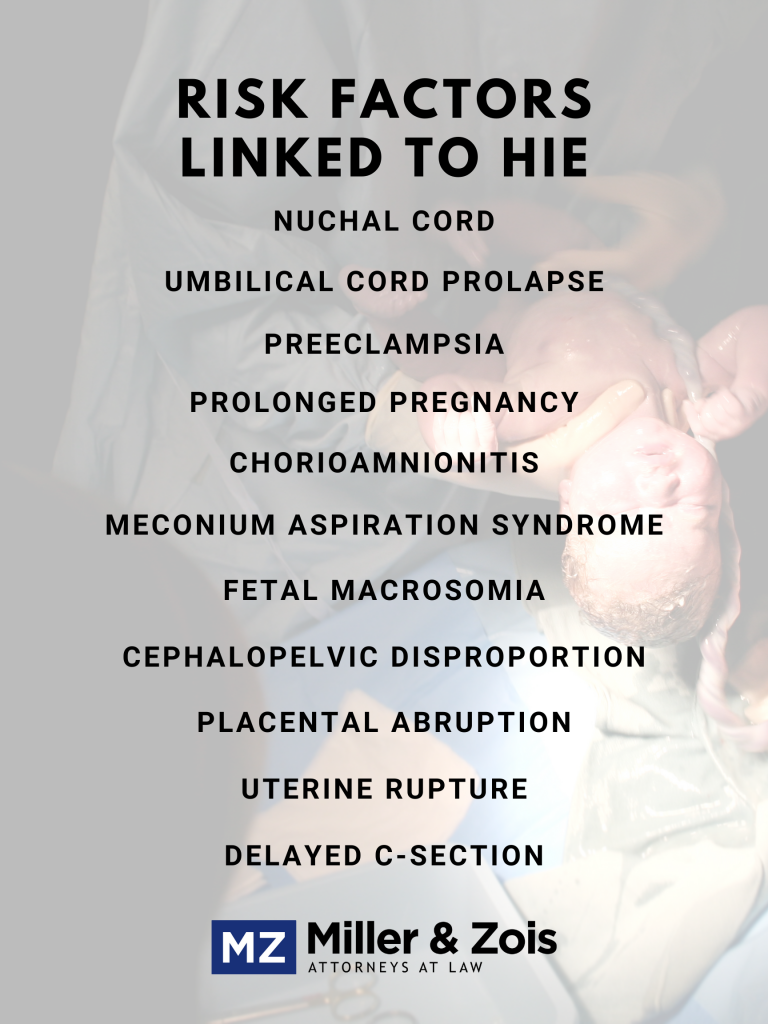
- An umbilical cord prolapse occurs when the umbilical cord enters the cervix/birth canal with or before the baby. The prolapsed cord becomes trapped and squeezed between the baby and the mother’s pelvis. The pressure put on the cord may slow or completely stop the blood flow to the baby. Cord prolapses are obstetrical emergencies that necessitate immediate delivery, usually via C-section.
- Preeclampsia: This condition can increase a baby’s risk of developing HIE. It occurs when a pregnant woman experiences acute high blood pressure during the latter stages of pregnancy. This can cause decreased blood flow to her baby because of damage or constriction to the placental vessels.
- Prolonged pregnancy: A post-term pregnancy, also known as a prolonged pregnancy, can cause HIE. They are pregnancies with a gestation period beyond 40 weeks, the standard gestation period. When the gestation period goes beyond 40 weeks, the placenta deteriorates and the amniotic fluid levels are reduced. Post-term pregnancies run the risk of the baby becoming too large. This may cause a difficult delivery that increases the HIE risk.
- Chorioamnionitis: Chorioamnionitis is an infection that inflames the placenta and fetal membranes. This can lead to premature rupturing of the amniotic sac and chorionic, which is supposed to happen during birth. Known as the prelabor, or premature, rupture of the membranes (PROM), it can affect lung development. Underdeveloped lungs may cause oxygen deprivation and HIE.
- Meconium aspiration syndrome: Meconium aspiration syndrome (MAS) occurs when a newborn baby experiences breathing complications. Meconium is a combination of amniotic fluid and a newborn’s fecal matter. Around childbirth, babies may inhale this material. This can lead to respiratory problems that can deprive the baby of oxygen and HIE.
- Fetal Macrosomia: Macrosomia occurs when the baby is too large to pass through the mother’s pelvis. Labor can be prolonged, which can be dangerous because the more contractions the baby has to withstand, the oxygen flow becomes limited. Doctors may have to result to forceps or vacuum extractors to pull out the baby. However, these tools may lead to head trauma, hemorrhages, and HIE.
- Cephalopelvic disproportion: Cephalopelvic disproportion (CPD) happens when the baby’s head is too large. It can lead to similar complications as macrosomia, such as prolonged labor.
- Placental abruption: Placental abruption happens when the placenta separates from the uterus’ inner wall during pregnancy. It may also completely or partially cut off blood supply from the placenta and the umbilical cord. This can cause internal bleeding for the mother and oxygen deprivation to the baby.
- Uterine rupture: A uterine rupture occurs when there is an open tear in the uterus. This could lead to the unborn baby being expelled into their mother’s abdomen. This usually happens to a mother who has previously undergone uterine surgery or a C-section birth. A torn uterus can also cause significant blood loss that results in oxygen deprivation to the baby. The uterine rupture can also result in both the placenta and umbilical cord become cut from circulation. Having a vaginal birth after C-section (VBAC) increases a mother’s risk of having her uterus tear open.
- Delayed C-section: Emergency C-sections occur as a response to risky childbirths. They should usually take about 5 to 30 minutes. Any longer than 30 increases the birth injury risk. Sometimes, doctors not properly trained to handle an emergency C-section or do not properly recognize fetal distress signs.
Hypoxic-Ischemic Encephalopathy Verdicts and Settlements
YEAR / STATE
CASE / INJURY SUMMARY
RESULT
2019 – Washington
A baby girl suffered hypoxic-ischemic encephalopathy during her delivery. As a result, she suffered permanent brain damage. The girl, now four years old, was cognitively impaired, motor functionally impaired, non-verbal, and not potty trained. Her family alleged that the hospital staff’s negligence caused her permanent injuries. They claimed the hospital failed to detect fetal distress and wrongly tracked the mother’s heart rate with the fetal heart monitor. The family argued that had fetal distress been timely detected, the hospital staff could have prevented brain damage by ordering an emergency C-section. A jury awarded a $23,900,000 verdict.
$23,900,000 – Verdict
2019 – Illinois
A baby girl suffered hypoxic-ischemic encephalopathy after being vaginally delivered. She developed cerebral palsy, mental deficits, impaired motor skills, and emotional trauma. Her mother claimed the physician failed to timely track the fetal heart monitor, failed to detect excessive uterine activity, failed to discontinue Pitocin, and failed to timely perform a C-section. This case settled for $14,000,000.
$14,000,000 – Verdict
2019 – Pennsylvania
A baby boy was born with hypoxic-ischemic encephalopathy, causing significant brain damage. He developed cerebral palsy, hearing loss, vision loss, and dystonia. Because of his condition, he required lifelong in-home care. His family claimed the hospital staff failed to timely admit his mother, improperly assessed her preeclampsia, failed to timely treat a placental abruption, and failed to timely order a C-section. This case settled for $3,500,000.
$3,500,000 – Settlement
2019 – Illinois
An expectant mother presented to the hospital with a membrane rupture at 28 weeks. The hospital staff performed tests that appeared to reveal no membrane rupture. They immediately discharged the woman. Twenty-eight hours later, the woman’s daughter was born via an emergency C-section. The baby girl sustained hypoxic-ischemic encephalopathy, which developed into cerebral palsy. Her mother alleged that the hospital staff’s negligence caused her permanent injuries. She claimed the hospital staff failed to perform additional tests to rule out membrane ruptures. This case settled for $12,000,000.
$12,000,000 – Settlement
2019 – California
A baby boy was born with hypoxic-ischemic encephalopathy. His family alleged that the hospital staff’s negligent care caused his permanent injuries. This case settled for $1,000,000.
$1,000,000 – Settlement
2019 – Massachusetts
A baby boy developed hypoxic-ischemic encephalopathy at birth. As a result, he sustained cerebral palsy, cortical blindness, nystagmus, esotropia, and quadriplegia. His mother alleged that the traveling nurse’s negligence caused his permanent injuries. She claimed she failed to monitor the fetal heart rate, failed to detect fetal distress, prolonged the second stage of labor, and failed to order an emergency C-section. The woman also alleged that the nurse deleted her medical records that determined how her son suffocated at birth. The nurse and hospital denied liability, arguing that they provided reasonable care. A jury ruled in the woman’s favor and awarded $30,550,000.
$30,550,000 – Verdict
Contact Miller & Zois About HIE and Birth Injuries
HIE and other birth injuries involving oxygen deprivation are frequently related to negligent medical care during labor and delivery. Contact the birth injury lawyers at Miller & Zois to find out if you have a malpractice case for your child’s brain injury. Call us at 800-553-8082 or contact us online.
 Maryland Medical Malpractice Attorney Blog
Maryland Medical Malpractice Attorney Blog

